Enteric Hyperoxaluria
Enteric Hyperoxaluria (EH) is caused by the increased absorption of oxalate from foods in the digestive tract (also called the gut or intestines). This leads to high levels of oxalate in the urine. EH may be acquired as a result of certain weight loss surgeries or in inflammatory bowel disease including Crohn’s disease, cystic fibrosis or chronic pancreatitis. Excess oxalate in the urine may lead to recurring kidney stones, chronic kidney disease or kidney failure. Symptoms vary but may include kidney stones, loose stools, or weight loss.

Symptoms
The symptoms of Enteric Hyperoxaluria may vary depending on the severity of the condition and the underlying cause, however the most common symptoms of EH are shown here:


Symptoms
The symptoms of Enteric Hyperoxaluria may vary depending on the severity of the condition and the underlying cause, however the most common symptoms of EH are shown here:


Enteric Hyperoxaluria FAQs
Thanks to feedback from experts and from those affected by Enteric Hyperoxaluria, The OHF is pleased to provide Frequently Asked Questions about EH. While these questions are intended to be a helpful resource, each individual is unique. To help minimize fat malabsorption which may be causing hyperoxaluria, it is recommended that you work with your physician and a registered dietitian to lower fat intake, to add calcium into your diet, and also to lower your oxalate intake from food, based upon your current diet and lab results.
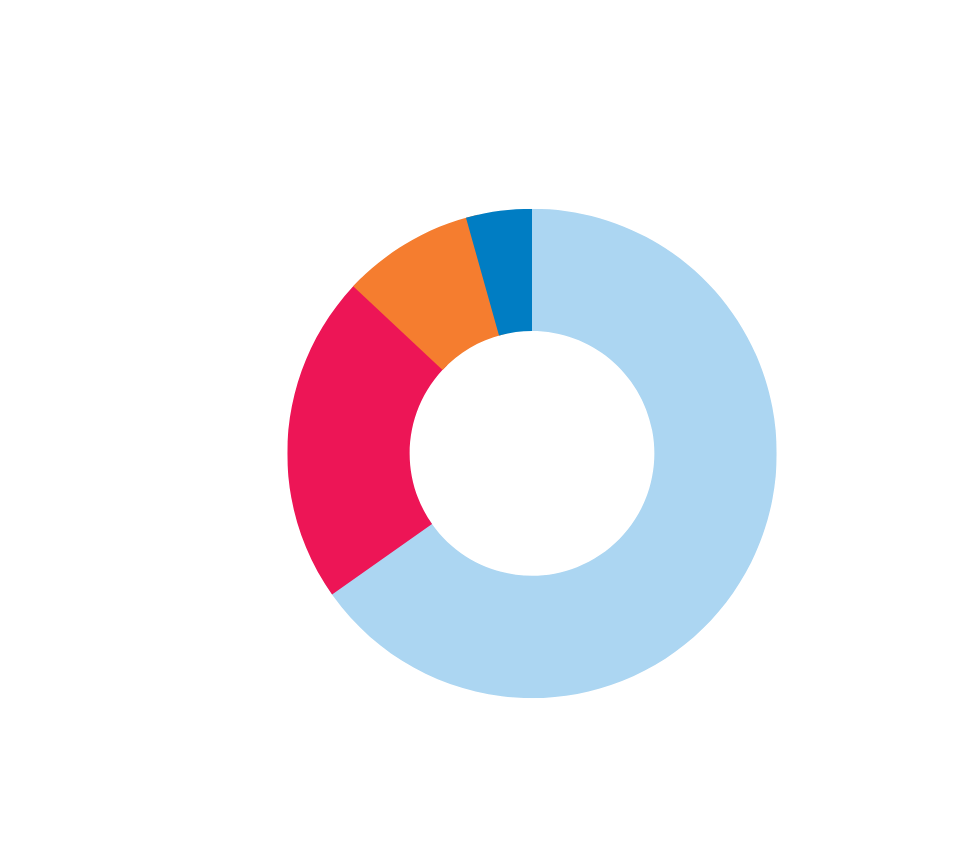
The prevalence of enteric hyperoxaluria is not well established, and estimates vary depending on the underlying condition that causes it. The most common causes can be seen here however, it is considered to be a relatively rare condition.
It is worth noting that enteric hyperoxaluria can also occur in people without any known underlying conditions that cause their fat malabsortion and who lack any apparent symptoms. The prevalence of these types of cases is not well established.

Causes of Enteric Hyperoxaluria
Some types of bariatric surgery, for example gastric bypass surgery, lead to decreased absorption of nutrients in the intestine or “malabsorption”. This malabsorption may increase the risk of Enteric Hyperoxaluria.
Currently the most common cause of Enteric Hyperoxaluria in western countries is malabsorption after bariatric surgery.
Enteric Hyperoxaluria diagnosed after bariatric surgery is a result of malabsorption caused by the surgery in order to promote weight loss, and does not have an inherited or genetic cause.
Although a high oxalate diet alone can lead to hyperoxaluria, diet is not a cause of Enteric Hyperoxaluria. However, a higher oxalate, lower calcium, or higher fat diet can make EH worse.
In the absence of malabsorption, oxalate binds to calcium in the gastrointestinal (GI) tract and is then eliminated through solid waste. However, in the case of Enteric Hyperoxaluria, fat malabsorption causes fat to remain in the GI tract instead of being absorbed by the body. The fat is therefore capable of binding to calcium within the gut. As a result, oxalate in the gut is unable to bind to calcium. Instead, it is absorbed by the body, enters the bloodstream, and raises oxalate levels. This elevation in oxalate levels leads to symptoms associated with Enteric Hyperoxaluria.
Medical care for Enteric Hyperoxaluria patients
It is recommended that you work with a team of health care providers, which may include specialists in intestinal disorders (gastroenterologists), specialists in kidney stones and kidney disease (nephrologists), and registered dieticians. Dietary management is an important component of care and includes lowering fat intake, adding calcium into your diet, and lowering your oxalate intake. Your primary care provider should also be a part of your health care team.
Many patients with EH find it extremely helpful to work closely with a dietician who is familiar with metabolic kidney stone disease.
Many but not all bariatric surgeons are aware of the risk for EH after bariatric surgery. The OHF is working to bring more bariatric surgeons, and members of their teams, into the conversation regarding hyperoxaluria to continue improving awareness of and treatment for Enteric Hyperoxaluria.
Regular visits with your kidney specialist are important to manage stones and to preserve kidney function. The frequency depends upon your specific circumstances and should be discussed with your kidney specialist.
Enteric Hyperoxaluria Treatment
The OHF has worked with dietary experts, and experts in primary and enteric hyperoxaluria care and research to develop a resource for oxalate levels in many common foods and beverages. This resource was compiled through extensive review of evidence based analysis of oxalate levels in food products and is available here.
High levels of fluid intake are very important. If you have advanced chronic kidney disease or are on dialysis, check with your provider for the amount of daily fluid intake appropriate for you.
Your urine oxalate should be monitored regularly. The frequency depends on your individual situation, but most providers monitor urine oxalate at minimum on an annual basis. Urine oxalate may need to be checked more often, especially if diet or medications are being changed, and should be determined by your healthcare provider. We encourage you to discuss this question with your care team.
Speak to your dietitian about putting together a balanced diet that is appropriate for your Enteric Hyperoxaluria. This may include lowering oxalate intake, increasing calcium, and reducing fat intake.
Your diet is highly important if you are on dialysis and must be individualized to manage both the Enteric Hyperoxaluria and your kidney disease.