What is Hyperoxaluria?
Hyper
(too much)
oxal
(oxalate)
uria
(in the urine)
Hyperoxaluria is a condition in which you have too much oxalate in your urine. Oxalate in a natural chemical in your body, and it’s also found in certain types of food. But too much oxalate in your body can cause serious problems. High levels of oxalate are toxic because oxalate cannot be broken down by the body and accumulates in the kidneys that may cause kidney stones. The long term health of your kidneys depends on early diagnosis and prompt treatment of hyperoxaluria.

Are There Different Types of Hyperoxaluria?
There are several types:

Primary Hyperoxaluria
Primary Hyperoxaluria (PH) is a genetic disease— you are born with it. It can present at any age and at any time. PH often goes underdiagnosed and is misdiagnosed. Recurrent kidney stones in adults or any kidney stone in a child is usually the most common sign that you might have PH. Visit our page here.

Enteric hyperoxaluria

Dietary hyperoxaluria
Dietary Hyperoxaluria is a result of eating large quantities of foods high in oxalate.

IDIOPATHIC (UNKNOWN) hyperoxaluria
Idiopathic hyperoxaluria is a type of hyperoxaluria where the cause is unknown. It means that the body produces or absorbs too much oxalate, which can lead to problems like kidney stones and urinary tract issues.
What Causes Primary Hyperoxaluria (PH)?
PH is a family of rare, genetic liver disorders that can damage the kidneys. The liver normally makes proteins, called enzymes, that prevent the body from making too much oxalate. In PH, the liver doesn’t create enough of this enzyme, or the enzyme doesn’t work properly.
PH1
AGXT
genetic mutation
AGXT
enzyme deficiency
PH2
GRHPR
genetic mutation
GR/HPR
enzyme deficiency
PH3
HOGA1
genetic mutation
HOGA1
enzyme deficiency
Symptoms
Although kidney stones are the most common and often the first symptom of hyperoxaluria, not all individuals with hyperoxaluria will have kidney stones. If you experience the below signs and symptoms, you should further investigate to understand the cause, because it could be hyperoxaluria:
- High levels of oxalate
- Urinary tract infection
- Blood in the urine
- Kidney stones as a child, even only 1
- Failure to thrive (not growing adequately as a baby
- Recurrent kidney stones
- Nephrocalcinosis (finding crystals in kidney tissue)
- Kidney failure
Life Stage Manifestations
| Infancy | Childhood/Adolescence/Adulthood |
|---|---|
| Insufficient weight gain | Multiple kidney stones |
| Formation of kidney stones | Progressive kidney stones (including kidney failure) |
| Early end-stage renal failure | Multi-organ dysfunction |
Prevalence of Hyperoxaluria
Approximately 1 to 3 of every million people have Primary Hyperoxaluria (PH). Type 1 is the most common form, accounting for approximately 80% of cases. Types 2 and 3 each account for about 10% of cases
The prevalence of Enteric Hyperoxaluria (EH) has been estimated at 5-24% of all patients with gastrointestinal diseases associated with malabsorption. EH is a frequent complication of inflammatory bowel diseases (IBD), ileal resection and Roux-en-Y gastric bypass (RYGB) and is well-known to cause kidney stones, and nephrocalcinosis. EH can also contribute to chronic kidney disease (CKD) and kidney failure.
Inheritance and Genetics
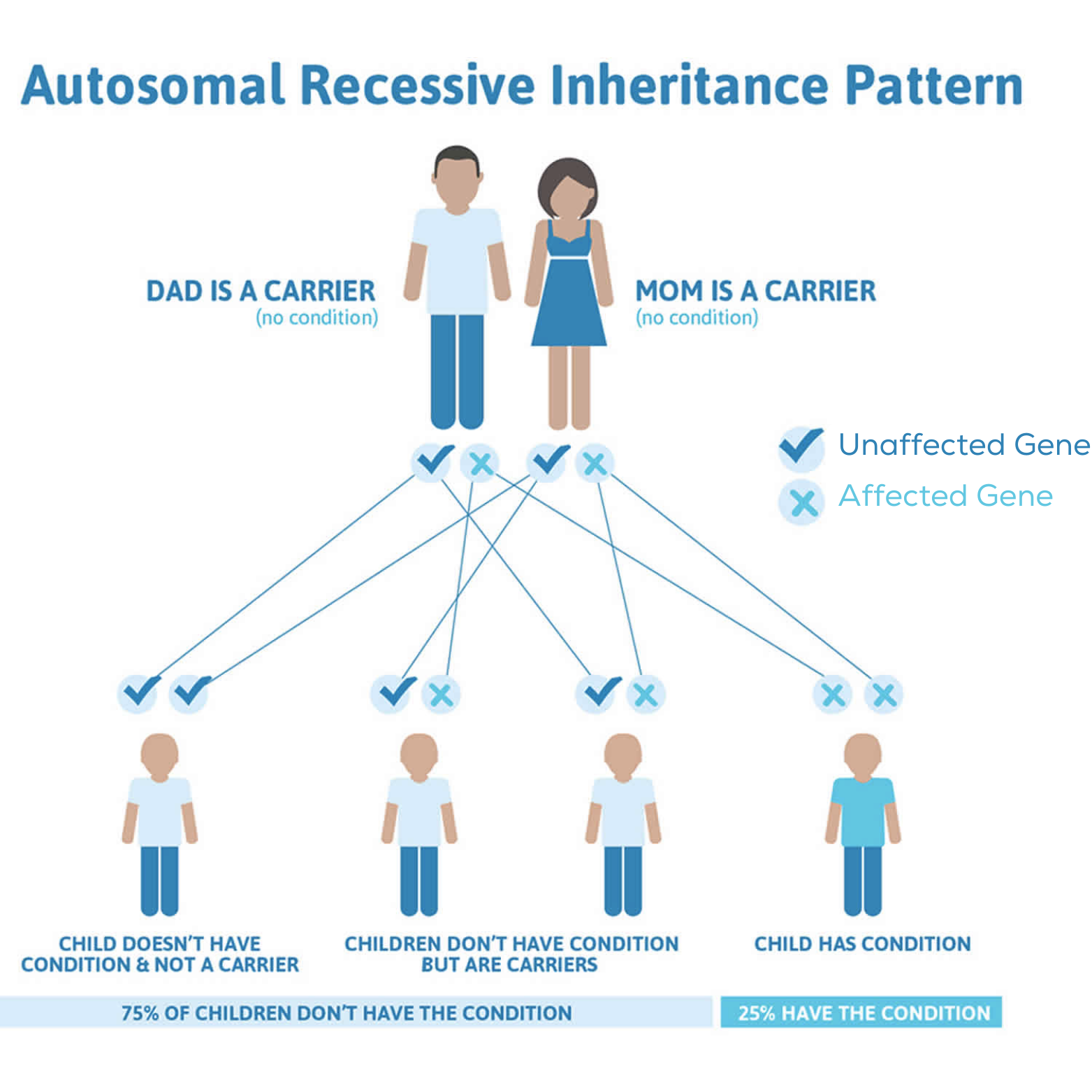
A genetic disorder is the result of changes known as pathologic variants in an individual’s DNA. A pathologic variant is a change or “spelling” mistake in the letters of DNA that tell the body how to produce a protein. This section of DNA that contains the instructions for a specific protein is known as a gene.
We have two copies of each gene, one inherited from each parent. PH is inherited in an autosomal recessive pattern, meaning that an affected individual must inherit a pathologic variant or copy of the gene from each parent. The pathologic genetic variants that cause PH control the production of 3 different proteins found primarily in the liver that cause PH1, PH2 and PH3.
Current and Future Treatment Options
Patients with all types of hyperoxaluria are managed by very large volumes of daily fluid intake and surgery to remove recurrent kidney stones. Untreated forms of the disease lead to progressive kidney damage and other systemic complications. Patients with advanced kidney disease may require intensive dialysis to help filter waste products, including oxalate, from their blood and may require a kidney or dual liver/kidney transplant, an invasive procedure associated with high-risk outcomes and life-long immunosuppression.
Currently, there is one approved therapy for patients with PH1. Having treatment for those with PH1 is encouraging, but there is still much more work to do. OHF is forging ahead with great energy and fervor to find effective treatments and a cure for all patients living with all primary and enteric hyperoxaluria. Read more about the approved therapy and ongoing clinical trials on the OHF website.
